The global demand for medical consumables, particularly precision devices such as multisample needles, continues to expand amid rising diagnostic testing volumes and advancements in blood collection technology. According to a 2023 report by Mordor Intelligence, the global needle and syringe market was valued at USD 22.8 billion and is projected to grow at a CAGR of 8.4% from 2023 to 2028, driven by increasing chronic disease prevalence, geriatric population growth, and expanded healthcare access in emerging economies. This growth is mirrored in the specialized segment of multisample needles—critical tools used in clinical laboratories for efficient, multi-vial blood collection—where accuracy, safety, and ergonomics are paramount. As healthcare systems prioritize infection control and workflow efficiency, the need for high-quality multisample needles has intensified, spurring innovation among leading medical device manufacturers. Based on market presence, product quality, regulatory compliance, and technological advancement, the following six companies have emerged as key players shaping the future of multisample needle production worldwide.
Top 6 Multisample Needle Manufacturers 2026
(Ranked by Factory Capability & Trust Score)
#1 Terumo Medical Products
Domain Est. 2007
Website: terumotmp.com
Key Highlights: Terumo Medical Care Solutions is a leading manufacturer of injection and infusion therapy devices that help clinicians consistently perform at their very best….
#2 Sol
Domain Est. 1996
Website: cardinalhealth.com
Key Highlights: The Sol-M® Multi-Sample Blood Collection Needles allow for the collection of blood into multiple vacuum collection tubes during a single venipuncture….
#3 Multi-Sample Blood Collection Needles, Sharps Safety
Domain Est. 1997
Website: icumed.com
Key Highlights: Multi-Sample Blood Collection Needles from ICU Medical are available in a wide range of sizes and can be used with Venipuncture Needle-Pro™ safety holders….
#4 BOENMED® Multi Sample Needle For Blood Collection, with luer …
Domain Est. 2006
Website: boenmedical.com
Key Highlights: The Multi Sample Needle can be used to draw blood directly from the vein into vacuum collection tubes to prevent exposure. Latex free, multi-sample needles ……
#5 SOL-M Multi-Sample Needle 21G x 1″
Domain Est. 2008
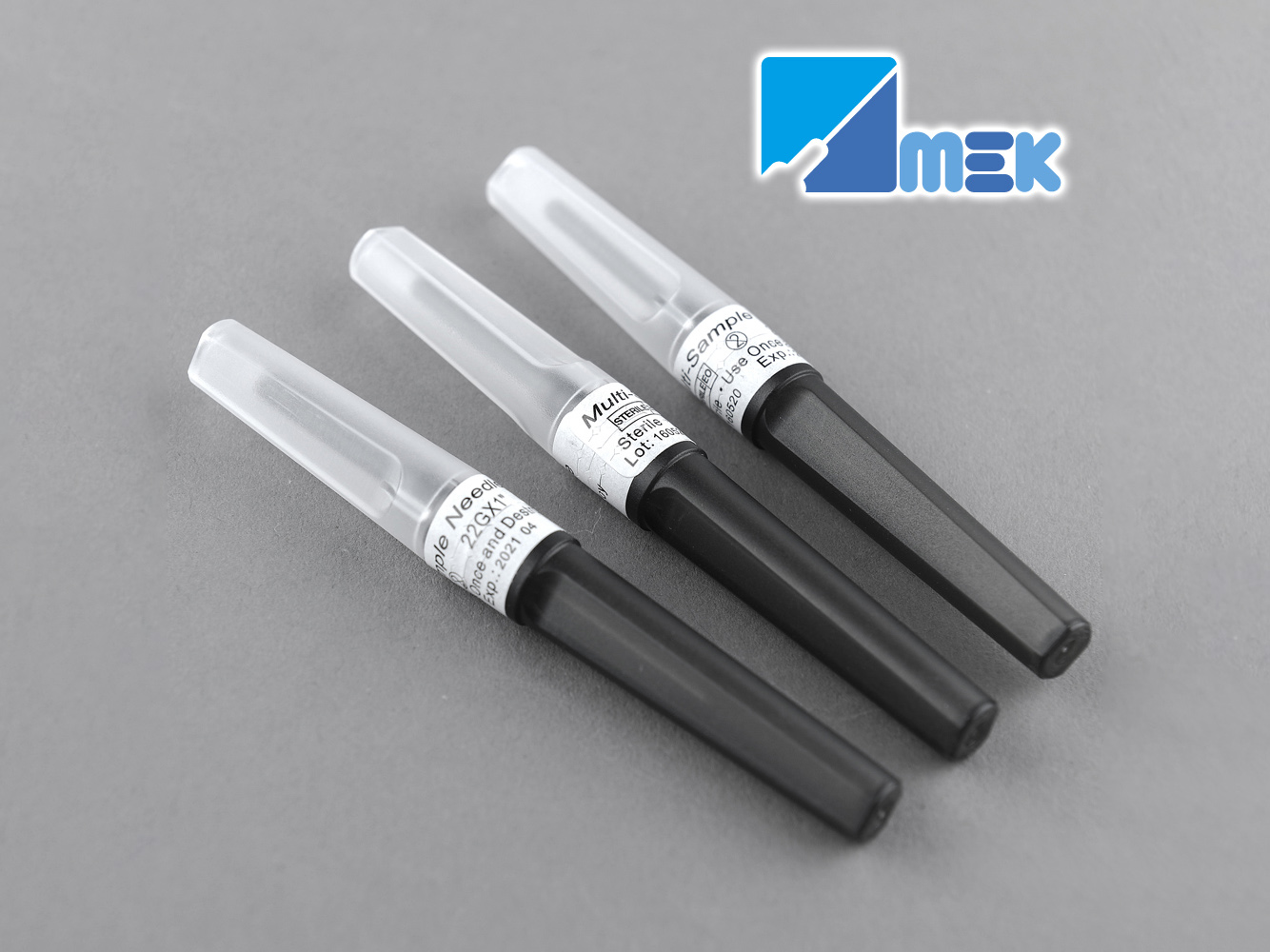
#6 Blood Collection Needle (Multi Sample Needle)
Domain Est. 2011
Expert Sourcing Insights for Multisample Needle

H2: Projected 2026 Market Trends for Multisample Needles
The multisample needle market is poised for significant evolution by 2026, driven by converging forces of technological advancement, shifting healthcare demands, and regulatory dynamics. Here’s a breakdown of key trends expected to shape the landscape:
-
Accelerated Adoption of Safety-Engineered Designs:
- Mandates & Regulations: Global expansion of safety device legislation (building on US OSHA, EU directives) will mandate near-universal adoption of safety-engineered multisample needles by 2026. This is the single most significant driver.
- Passive Safety Dominance: Passive safety mechanisms (automatic retraction, shielding upon syringe disengagement) will become the standard, minimizing reliance on user activation and maximizing compliance. Active safety devices will face increasing pressure.
- Integrated Safety Systems: Needle safety will be increasingly integrated into broader phlebotomy safety systems, including holders, tubes, and training protocols.
-
Technological Innovation Focus:
- Enhanced Patient Comfort & Ease of Use: Development will prioritize smaller gauge needles (e.g., 23G, 25G), improved bevel designs, and optimized flow dynamics to reduce pain, bruising, and hemolysis, especially for challenging draws (geriatric, pediatric, obese patients).
- Material Science Advancements: Wider use of biocompatible, low-friction coatings (e.g., PTFE, silicon) to improve blood flow, reduce clotting, and enhance patient comfort. Exploration of novel materials for durability and safety.
- “Smart” Features (Emerging): Early adoption of features like visual flow indicators or integrated sensors (for clot detection or fill level) may begin, particularly in premium segments, though widespread implementation by 2026 is likely limited.
-
Market Consolidation & Strategic Partnerships:
- Increased M&A Activity: Larger players (BD, Terumo, Greiner Bio-One, Becton Dickinson) will likely acquire innovative smaller companies or niche safety technology developers to strengthen portfolios and gain market share.
- Supplier Consolidation: Healthcare systems, driven by cost pressures and supply chain efficiency, will favor suppliers offering comprehensive phlebotomy portfolios (needles, tubes, holders, safety systems), leading to vendor consolidation.
- Strategic Alliances: Partnerships between needle manufacturers and tube/holder companies to offer integrated, optimized safety solutions will become more common.
-
Growth in Alternative Venipuncture Settings:
- Home Healthcare & Point-of-Care (POC): Expansion of home-based blood collection (e.g., for chronic disease monitoring, clinical trials) and POC testing (clinics, ambulatory surgery centers) will drive demand for user-friendly, highly safe multisample systems suitable for non-traditional settings.
- Emerging Markets: Significant growth potential in Asia-Pacific, Latin America, and Africa, fueled by improving healthcare infrastructure, rising awareness of blood-borne pathogens, and increasing adoption of safety standards. Affordability and supply chain reliability will be key challenges.
-
Heightened Focus on Hemolysis Reduction & Sample Quality:
- Clinical Demand: Growing awareness of hemolysis as a major cause of pre-analytical errors and lab rejected samples will push innovation towards designs minimizing shear stress and turbulence during blood draw (e.g., optimized luer connections, flow control).
- Standardization Pressure: Laboratories and accreditation bodies (like CLSI) will continue to emphasize protocols and tools (including needle choice) that minimize sample degradation.
-
Sustainability & Environmental Considerations:
- Material Reduction: Design efforts will focus on minimizing plastic usage without compromising safety or function.
- Recyclability: Exploration of more easily recyclable materials and design for disassembly (e.g., separating sharps from plastic components) will gain traction, driven by institutional sustainability goals and potential future regulations.
- Packaging Optimization: Reduction of primary and secondary packaging waste will be a focus area.
-
Pricing Pressures & Value-Based Procurement:
- Cost Containment: Healthcare providers will continue to exert strong pressure on prices. Suppliers will need to demonstrate clear value beyond the initial cost – emphasizing reduced needlestick injuries (lowering costly OSHA incidents), reduced sample rejection rates (saving on re-draws and lab costs), and improved workflow efficiency.
- Total Cost of Ownership (TCO): Procurement decisions will increasingly be based on TCO analysis, factoring in safety performance, sample quality, and labor efficiency, not just unit price.
Conclusion for 2026:
The multisample needle market in 2026 will be defined by safety, integration, and value. Passive safety will be non-negotiable. Innovation will focus on enhancing patient experience, sample integrity, and operational efficiency within consolidated supply chains. Success will depend on manufacturers’ ability to offer reliable, safe, high-quality, and cost-effective solutions that demonstrably reduce risks and costs across the entire blood collection and testing pathway, while also addressing emerging demands from alternative care settings and environmental sustainability.

Common Pitfalls When Sourcing Multisample Needles: Quality and Intellectual Property Concerns
Sourcing multisample needles—commonly used in medical, diagnostic, and laboratory applications—requires careful evaluation to avoid critical issues related to both product quality and intellectual property (IP) rights. Overlooking these aspects can lead to regulatory non-compliance, compromised patient safety, legal disputes, and reputational damage. Below are key pitfalls to watch for in both domains.
Quality-Related Pitfalls
1. Inconsistent Manufacturing Standards
Many suppliers, especially those in less-regulated markets, may not adhere to international quality standards such as ISO 13485 or FDA QSR (Quality System Regulation). This can result in variability in needle sharpness, wall thickness, and sterility—critical factors that impact performance and safety.
2. Use of Substandard Materials
Low-cost suppliers may use inferior-grade stainless steel or non-compliant lubricants, leading to increased risk of needle breakage, corrosion, or adverse tissue reactions. Always verify material certifications and biocompatibility testing (e.g., ISO 10993).
3. Inadequate Sterilization and Packaging
Improper sterilization processes or compromised packaging integrity can introduce contamination. Ensure the supplier provides valid sterility assurance level (SAL) documentation and validated packaging methods (e.g., EO or gamma irradiation).
4. Lack of Traceability and Documentation
Reputable manufacturers offer full traceability, including lot numbers, Certificates of Conformance (CoC), and batch testing reports. A lack of such documentation is a red flag indicating potential quality control deficiencies.
5. Insufficient Validation and Testing
Some suppliers may not conduct proper functional testing—such as bevel quality, penetration force, or leakage checks—leading to undetected defects. Request evidence of design and process validation per ISO 14155 or equivalent standards.
Intellectual Property-Related Pitfalls
1. Risk of Infringing Patented Designs
Multisample needles may incorporate proprietary features (e.g., specialized bevel geometry, safety mechanisms, or hub designs) protected by utility or design patents. Sourcing from manufacturers that replicate patented technologies without licensing exposes your company to infringement lawsuits.
2. Unverified Supplier IP Compliance
Suppliers may claim their products are “generic” or “patent-free” without providing proof. Always conduct due diligence by performing patent landscape analyses or working with IP counsel to confirm freedom-to-operate (FTO) in your target markets.
3. Copying Proprietary Product Features
Even if a needle appears functionally similar, minor design differences might still infringe on existing IP. Reverse engineering without proper legal clearance can lead to costly litigation and product recalls.
4. Ambiguous Ownership in Custom Designs
If you commission a custom multisample needle design, ensure the contract clearly assigns IP rights to your organization. Without a written agreement, the manufacturer may retain ownership or reuse the design for competitors.
5. Counterfeit or Gray Market Goods
Purchasing from unauthorized distributors increases the risk of receiving counterfeit products that mimic branded, patented designs. These not only pose safety risks but also expose your business to contributory infringement claims.
Mitigation Strategies
- Conduct Supplier Audits: Perform on-site or third-party audits to verify quality systems and manufacturing practices.
- Require Full Documentation: Insist on CoAs, CoCs, sterilization records, and biocompatibility data.
- Perform IP Due Diligence: Engage IP professionals to review relevant patents and conduct FTO assessments.
- Use Legally Binding Contracts: Include IP ownership clauses, indemnification for infringement, and quality compliance terms.
- Source from Reputable, Certified Suppliers: Prefer vendors with ISO 13485 certification and a proven track record in medical device components.
By proactively addressing these quality and IP pitfalls, organizations can ensure reliable supply chains, regulatory compliance, and protection against legal and operational risks when sourcing multisample needles.

Logistics & Compliance Guide for Multisample Needle
Product Overview
The Multisample Needle is a medical device designed for venipuncture procedures, enabling the collection of multiple blood samples into evacuated tubes without removing the needle from the patient’s vein. It is commonly used in clinical settings to improve efficiency, reduce patient discomfort, and maintain sample integrity. This guide outlines key logistics considerations and regulatory compliance requirements for the safe distribution, handling, and use of multisample needles.
Intended Use & Classification
Multisample needles are classified as Class II medical devices under regulatory frameworks such as the U.S. FDA 510(k) clearance and the EU Medical Device Regulation (MDR) 2017/745. Their intended use includes venous blood collection in healthcare environments, typically in conjunction with blood collection tubes and holders. Device labeling must clearly state the intended use, contraindications, and warnings to ensure proper application.
Regulatory Compliance Requirements
Manufacturers and distributors must adhere to region-specific regulatory standards. In the United States, compliance with FDA 21 CFR Parts 803 (Medical Device Reporting), 806 (Correction and Removals), and 820 (Quality System Regulation) is mandatory. In the European Union, CE marking under MDR requires a technical documentation file, conformity assessment by a Notified Body, and adherence to post-market surveillance obligations. Other markets (e.g., Canada, Australia, Japan) have similar registration and quality management system requirements.
Packaging & Labeling Standards
Multisample needles must be individually sterile-packaged using validated methods (e.g., ethylene oxide or gamma irradiation). Primary packaging should maintain sterility until point of use. Labels must include UDI (Unique Device Identifier), lot number, expiration date, sterility indication, and compliance markings (e.g., CE, FDA). Language-specific labeling may be required for international distribution. Tamper-evident features are recommended to ensure product integrity.
Storage & Handling Conditions
Store multisample needles in a dry, cool environment with temperatures between 15°C and 30°C (59°F to 86°F) and relative humidity below 60%. Avoid direct sunlight and exposure to extreme temperatures. Protect from physical damage during storage and transport. Do not use if packaging is compromised or past the expiration date. Follow manufacturer-recommended shelf life, typically 3–5 years from production.
Transportation & Distribution
Use validated shipping containers to maintain environmental conditions during transit. Employ cold chain logistics if required by regional regulations or product specifications. Ensure transport complies with IATA and IMDG regulations if shipping internationally, especially for air freight. Distributors must maintain traceability through lot tracking and temperature monitoring where applicable.
Import/Export Documentation
Accurate documentation is essential for cross-border movement. Required documents include commercial invoices, packing lists, certificates of conformity, certificates of free sale, and import permits. For the EU, an Authorized Representative must be designated. In the U.S., FDA prior notice of imported medical devices is required. Harmonized System (HS) codes (e.g., 9018.39) must be correctly applied to avoid customs delays.
Post-Market Surveillance & Vigilance Reporting
Manufacturers are responsible for monitoring device performance post-launch. Implement a robust post-market surveillance (PMS) system to collect and analyze complaints, adverse events, and field safety corrective actions (FSCAs). Report serious incidents to relevant authorities (e.g., FDA MedWatch, EUDAMED) within mandated timelines (e.g., 10–15 days in the EU). Maintain complaint handling and corrective action procedures per ISO 13485.
Quality Management System (QMS)
All stakeholders must operate under a certified QMS, such as ISO 13485:2016, covering design, manufacturing, distribution, and servicing. Regular internal audits, supplier controls, and management reviews are critical to ensure ongoing compliance. Documentation must be retained for at least the device’s shelf life plus an additional 2 years (region-dependent).
Training & User Competency
Only trained healthcare professionals should use multisample needles. Provide comprehensive instructions for use (IFU) in local languages. Distributors and healthcare facilities must ensure staff are trained in aseptic technique, needle safety, and proper disposal to minimize sharps injuries and contamination risks.
Environmental & Disposal Compliance
Dispose of used multisample needles as biohazardous waste in accordance with local regulations (e.g., OSHA Bloodborne Pathogens Standard in the U.S.). Use puncture-resistant sharps containers. Follow environmental guidelines for medical waste incineration or autoclaving. Consider sustainability in packaging design and lifecycle management.
In conclusion, sourcing a multisample needle requires careful consideration of several key factors to ensure safety, efficiency, and compatibility with existing phlebotomy procedures. It is essential to evaluate product quality, sterility, material composition (such as stainless steel gauge and needle design), and compliance with international standards (e.g., ISO, CE marking). Supplier reliability, cost-effectiveness, and consistent availability are also critical for maintaining uninterrupted clinical operations. Additionally, prioritizing features like patient comfort, ease of use for healthcare professionals, and safety mechanisms to prevent needlestick injuries can significantly enhance overall outcomes. Selecting the right multisample needle through a thorough sourcing process supports improved blood collection efficiency, patient satisfaction, and staff safety in clinical and laboratory environments.